Lobbying for our Clients: Valletta’s Trip to Capitol Hill
July 17, 2017
On the final day of HBMA’s 2017 Compliance Symposium, a few of us at The Valletta Group had the opportunity to meet with members of Congress to discuss various healthcare issues. It’s no secret that healthcare policy is currently in a state of volatility. In times of heated debate such as this, often only the most serious and divisive issues receive attention. Unfortunately, this can cause lesser-known, yet equally important issues to get overlooked.
Thus, the time is critical for RCM companies like ourselves to further relationships with our leaders and stand up for the policies that protect our clients and their patients. So when The Valletta Group and other HBMA members visited Capitol Hill, we spoke up for these lesser-known, bipartisan issues. These are the policies that help ensure a level playing field between insurance payers and physicians/patients.
Two of these issues are discussed below.

The Valletta Group’s Executive VP’s, Gilbert Johnston and Cal LaGroue, meet with United States Senator, Luther Strange.
Protecting our Providers: HIPAA Compliance Procedures
June 28, 2017
A few weeks ago, members of The Valletta Group attended the Healthcare Business Management Association’s (HBMA) Annual Compliance Symposium in Washington D.C. The event featured highly-informative lectures from various experts in the healthcare industry.
Compliance is a rather broad subject. Quite simply, it is the act of abiding by the governing rules and regulations of a particular industry. However, in the revenue cycle management (RCM) industry, certain aspects of compliance command much greater attention. At the forefront of most RCM insiders’ minds is the Healthcare Insurance Portability and Accountability Act (HIPAA) and more specifically, the privacy and security sections of Title II.
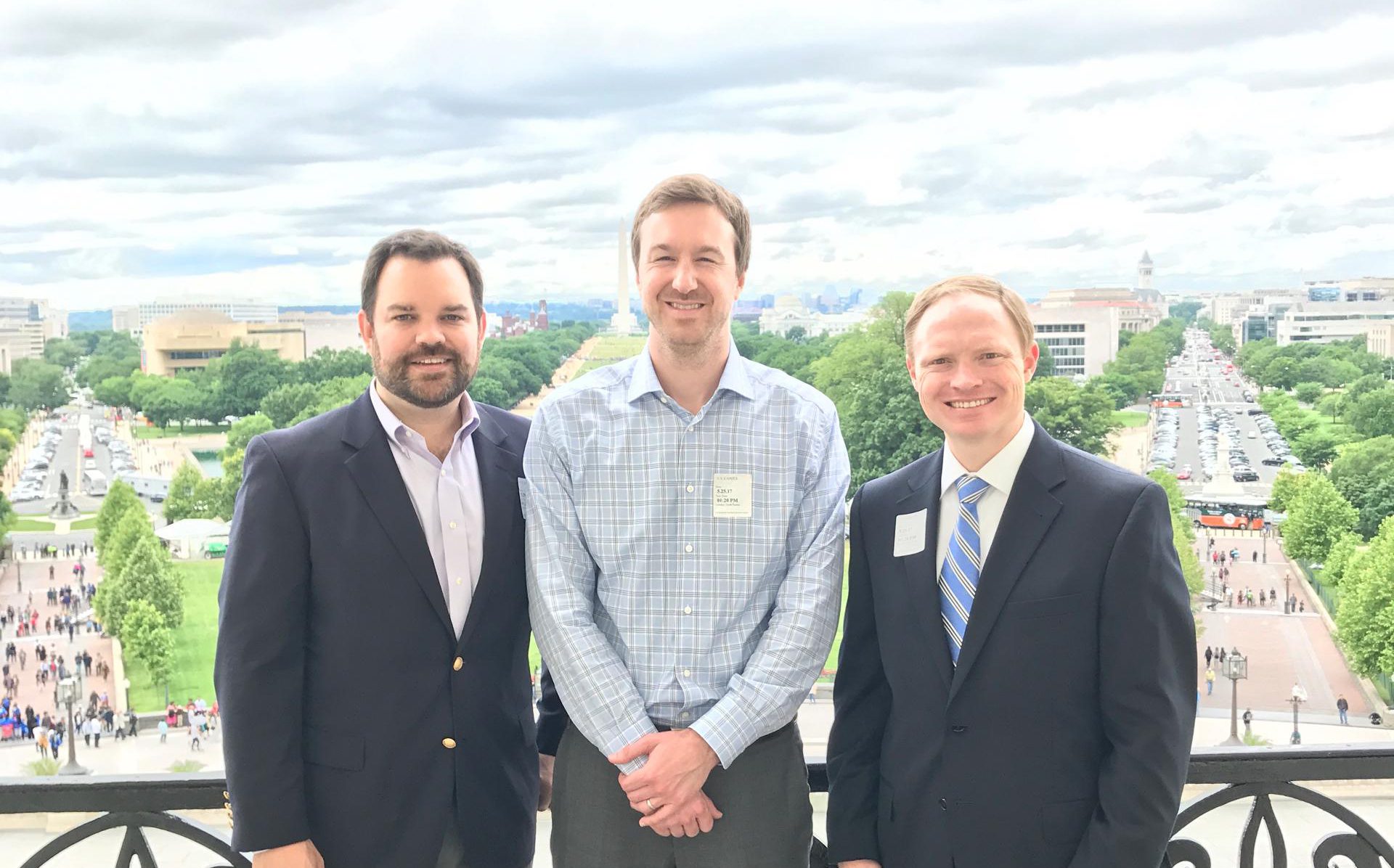
Gilbert Johnston, Jeff Bolar, and Cal LaGroue of The Valletta Group enjoying the view from the Senate majority leader’s private balcony.
Should I participate in the Quality Payment Program and MIPS?
May 15, 2017
The following information is provided by the Centers for Medicare & Medicaid Services:
You may have heard that the Centers for Medicare & Medicaid Services (CMS) is reviewing claims and letting practices know which clinicians should take part in the Merit-based Incentive Payment System (MIPS). MIPS is an important part of the new Quality Payment Program.
The Quality Payment Program works to make Medicare better by keeping patients at the center of healthcare while paying clinicians based on their performance. It replaces the Sustainable Growth Rate formula, which threatened clinicians participating in Medicare with potential payment cuts for 13 years. This program combines and streamlines many existing Medicare quality programs. It also gives new ways to improve care delivery by supporting and rewarding clinicians who:
- Find new ways to engage patients, families, and caregivers.
- Improve care coordination and population health management.
Valletta’s Commitment to Compliance
April 17, 2017
The Valletta Group is committed to doing all it can to protect its clients’ interests. When it comes to compliance, we are especially vigilant. That’s why we’ll once again be attending HBMA’s Annual Compliance Symposium. Each year, this event presents an opportunity to gain valuable education and insights, as well as an opportunity to discuss relevant issues with industry peers.